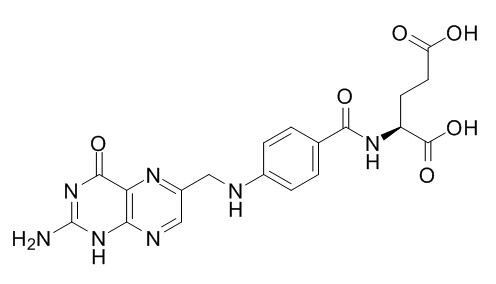
Folic acid
Folic acid supplementation improves arterial endothelial function in adults with relative hyperhomocystinemia, with potentially beneficial effects on the atherosclerotic process. Both local perfusion of 5-MTHF and supplementation with folic acid increase vasodilatation in ageing individuals through NO-dependent mechanisms. The combined use of enalapril and Folic acid significantly reduced the risk of first stroke, folic acid deficiency and homocysteine impaired DNA repair in hippocampal neurons and sensitized them to amyloid toxicity.
Inquire / Order:
manager@chemfaces.com
Technical Inquiries:
service@chemfaces.com
Tel:
+86-27-84237783
Fax:
+86-27-84254680
Address:
1 Building, No. 83, CheCheng Rd., Wuhan Economic and Technological Development Zone, Wuhan, Hubei 430056, PRC
Providing storage is as stated on the product vial and the vial is kept tightly sealed, the product can be stored for up to
24 months(2-8C).
Wherever possible, you should prepare and use solutions on the same day. However, if you need to make up stock solutions in advance, we recommend that you store the solution as aliquots in tightly sealed vials at -20C. Generally, these will be useable for up to two weeks. Before use, and prior to opening the vial we recommend that you allow your product to equilibrate to room temperature for at least 1 hour.
Need more advice on solubility, usage and handling? Please email to: service@chemfaces.com
The packaging of the product may have turned upside down during transportation, resulting in the natural compounds adhering to the neck or cap of the vial. take the vial out of its packaging and gently shake to let the compounds fall to the bottom of the vial. for liquid products, centrifuge at 200-500 RPM to gather the liquid at the bottom of the vial. try to avoid loss or contamination during handling.
University of Limpopo2016, 1777
Heliyon.2023, e12778.
Chem Biodivers.2023, 20(12):e202301461.
Asian Pac J Cancer Prev. 2020, 21(4):935-941.
J.Food Processing & Preservation2022, jfpp.16666
Molecules.2023, 28(13):4972.
Journal of functional foods2018, 171-182
Chulalongkorn University2024, ssrn.4716057.
Nutrients.2024, 16(19):3266.
Microb Biotechnol.2021, 14(5):2009-2024.
Related and Featured Products
J Neurosci. 2002 Mar 1;22(5):1752-62.
Folic acid deficiency and homocysteine impair DNA repair in hippocampal neurons and sensitize them to amyloid toxicity in experimental models of Alzheimer's disease.[Pubmed:
11880504]
Recent epidemiological and clinical data suggest that persons with low Folic acid levels and elevated homocysteine levels are at increased risk of Alzheimer's disease (AD), but the underlying mechanism is unknown.
METHODS AND RESULTS:
We tested the hypothesis that impaired one-carbon metabolism resulting from Folic acid deficiency and high homocysteine levels promotes accumulation of DNA damage and sensitizes neurons to amyloid beta-peptide (Abeta) toxicity. Incubation of hippocampal cultures in Folic acid-deficient medium or in the presence of methotrexate (an inhibitor of Folic acid metabolism) or homocysteine induced cell death and rendered neurons vulnerable to death induced by Abeta. Methyl donor deficiency caused uracil misincorporation and DNA damage and greatly potentiated Abeta toxicity as the result of reduced repair of Abeta-induced oxidative modification of DNA bases. When maintained on a Folic acid-deficient diet, amyloid precursor protein (APP) mutant transgenic mice, but not wild-type mice, exhibited increased cellular DNA damage and hippocampal neurodegeneration. Levels of Abeta were unchanged in the brains of folate-deficient APP mutant mice.
CONCLUSIONS:
Our data suggest that Folic acid deficiency and homocysteine impair DNA repair in neurons, which sensitizes them to oxidative damage induced by Abeta.
Clin Sci (Lond). 2015 Jul;129(2):159-67.
Folic acid supplementation improves microvascular function in older adults through nitric oxide-dependent mechanisms.[Pubmed:
25748442]
Older adults have reduced vascular endothelial function, evidenced by attenuated nitric oxide (NO)-dependent cutaneous vasodilatation. Folic acid and its metabolite, 5-methyltetrahydrofolate (5-MTHF), are reported to improve vessel function.
We hypothesized that (i) local 5-MTHF administration and (ii) chronic Folic acid supplementation would improve cutaneous microvascular function in ageing through NO-dependent mechanisms.
METHODS AND RESULTS:
There were two separate studies in which there were 11 young (Y: 22 ± 1 years) and 11 older (O: 71 ± 3 years) participants. In both studies, two intradermal microdialysis fibres were placed in the forearm skin for local delivery of lactated Ringer's solution with or without 5 mM 5-MTHF. Red cell flux was measured by laser-Doppler flowmetry. Cutaneous vascular conductance [CVC=red cell flux/mean arterial pressure] was normalized as percentage maximum CVC (%CVCmax) (28 mM sodium nitroprusside, local temperature 43°C). In study 1 after CVC plateaued during local heating, 20 mM NG-nitro-L-arginine methyl ester (L-NAME) was perfused at each site to quantify NO-dependent vasodilatation. The local heating plateau (%CVCmax: O = 82 ± 3 vs Y = 96 ± 1, P = 0.002) and NO-dependent vasodilatation (%CVCmax: O = 26 ± 6% vs Y = 49 ± 5, P = 0.03) were attenuated in older participants. 5-MTHF augmented the overall (%CVCmax = 91 ± 2, P = 0.03) and NO-dependent (%CVCmax = 43 ± 9%, P = 0.04) vasodilatation in older but not young participants. In study 2 the participants ingested Folic acid (5 mg/day) or placebo for 6 weeks in a randomized, double-blind, crossover design. A rise in oral temperature of 1°C was induced using a water-perfused suit, body temperature was held and 20 mM L-NAME was perfused at each site. Older participants had attenuated reflex (%CVCmax: O = 31 ± 8 vs Y = 44 ± 5, P = 0.001) and NO-dependent (%CVCmax: O = 9 ± 2 vs Y = 21 ± 2, P = 0.003) vasodilatation.
Folic acid increased CVC (%CVCmax = 47 ± 5%, P = 0.001) and NO-dependent vasodilatation (20 ± 3%, P = 0.003) in the older but not the young participants.
CONCLUSIONS:
Both local perfusion of 5-MTHF and supplementation with Folic acid increase vasodilatation in ageing individuals through NO-dependent mechanisms.
JAMA. 2015 Apr 7;313(13):1325-35.
Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial.[Pubmed:
25771069]
Uncertainty remains about the efficacy of Folic acid therapy for the primary prevention of stroke because of limited and inconsistent data.
To test the primary hypothesis that therapy with enalapril and Folic acid is more effective in reducing first stroke than enalapril alone among Chinese adults with hypertension.
METHODS AND RESULTS:
The China Stroke Primary Prevention Trial, a randomized, double-blind clinical trial conducted from May 19, 2008, to August 24, 2013, in 32 communities in Jiangsu and Anhui provinces in China. A total of 20,702 adults with hypertension without history of stroke or myocardial infarction (MI) participated in the study.
Eligible participants, stratified by MTHFR C677T genotypes (CC, CT, and TT), were randomly assigned to receive double-blind daily treatment with a single-pill combination containing enalapril, 10 mg, and Folic acid, 0.8 mg (n = 10,348) or a tablet containing enalapril, 10 mg, alone (n = 10,354).
The primary outcome was first stroke. Secondary outcomes included first ischemic stroke; first hemorrhagic stroke; MI; a composite of cardiovascular events consisting of cardiovascular death, MI, and stroke; and all-cause death.
During a median treatment duration of 4.5 years, compared with the enalapril alone group, the enalapril-Folic acid group had a significant risk reduction in first stroke (2.7% of participants in the enalapril-Folic acid group vs 3.4% in the enalapril alone group; hazard ratio [HR], 0.79; 95% CI, 0.68-0.93), first ischemic stroke (2.2% with enalapril-Folic acid vs 2.8% with enalapril alone; HR, 0.76; 95% CI, 0.64-0.91), and composite cardiovascular events consisting of cardiovascular death, MI, and stroke (3.1% with enalapril-Folic acid vs 3.9% with enalapril alone; HR, 0.80; 95% CI, 0.69-0.92). The risks of hemorrhagic stroke (HR, 0.93; 95% CI, 0.65-1.34), MI (HR, 1.04; 95% CI, 0.60-1.82), and all-cause deaths (HR, 0.94; 95% CI, 0.81-1.10) did not differ significantly between the 2 treatment groups. There were no significant differences between the 2 treatment groups in the frequencies of adverse events.
CONCLUSIONS:
Among adults with hypertension in China without a history of stroke or MI, the combined use of enalapril and Folic acid, compared with enalapril alone, significantly reduced the risk of first stroke. These findings are consistent with benefits from folate use among adults with hypertension and low baseline folate levels.
Acta Obstet Gynecol Scand. 2015 Jan;94(1):65-71.
Folic acid supplementation and methylenetetrahydrofolate reductase (MTHFR) gene variations in relation to in vitro fertilization pregnancy outcome.[Pubmed:
25283235]
To study Folic acid intake, folate status and pregnancy outcome after infertility treatment in women with different infertility diagnoses in relation to methylenetetrahydrofolate reductase (MTHFR) 677C>T, 1298A>C and 1793G>A polymorphisms. Also the use of Folic acid supplements, folate status and the frequency of different gene variations were studied in women undergoing infertility treatment and fertile women.
DESIGN:
Observational study.
SETTING:
University hospital.
POPULATION:
Women undergoing infertility treatment and healthy, fertile, non-pregnant women.
METHODS AND RESULTS:
A questionnaire was used to assess general background data and use of dietary supplements. Blood samples were taken to determine plasma folate and homocysteine levels, and for genomic DNA extraction. A comparison of four studies was performed to assess pregnancy outcome in relation to MTHFR 677 TT vs. CC, and 1298 CC vs. AA polymorphisms.
MAIN OUTCOME MEASURES:
Folic acid supplement intake, and plasma folate, homocysteine and genomic assays.
Women in the infertility group used significantly more Folic acid supplements and had better folate status than fertile women, but pregnancy outcome after fertility treatment was not dependent on Folic acid intake, folate status or MTHFR gene variations.
CONCLUSIONS:
High Folic acid intakes and MTHFR gene variations seem not to be associated with helping women to achieve pregnancy during or after fertility treatment.
J Am Coll Cardiol. 1999 Dec;34(7):2002-6.
Folic acid improves arterial endothelial function in adults with hyperhomocystinemia.[Pubmed:
10588216]
To evaluate whether oral Folic acid supplementation might improve endothelial function in the arteries of asymptomatic adults with hyperhomocystinemia.
Hyperhomocystinemia is an independent risk factor for endothelial dysfunction and occlusive vascular disease. Folic acid supplementation can lower homocystine levels in subjects with hyperhomocystinemia; however, the effect of this on arterial physiology is not known.
METHODS AND RESULTS:
Adults subjects were recruited from a community-based atherosclerosis study on healthy volunteers aged 40 to 70 years who had no history of hypertension, diabetes mellitus, hyperlipidemia, ischemic heart disease or family history of premature atherosclerosis (n = 89). Seventeen subjects (aged 54 +/- 10 years, 15 male) with fasting total homocystine levels above 75th percentile (mean, 9.8 +/- 2.8 micromol/liter) consented to participate in a double-blind, randomized, placebo-controlled and crossover trial; each subject received oral Folic acid (10 mg/day) and placebo for 8 weeks, each separated by a washout period of four weeks. Flow-mediated endothelium-dependent dilation (percent increase in diameter) of the brachial artery was assessed by high resolution ultrasound, before and after Folic acid or placebo supplementation.
Compared with placebo, Folic acid supplementation resulted in higher serum folate levels (66.2 +/- 7.0 vs. 29.7 +/- 14.8 nmol/liter; p < 0.001), lower total plasma homocystine levels (8.1 +/- 3.1 vs. 9.5 +/- 2.5 micromol/liter, p = 0.03) and significant improvement in endothelium-dependent dilation (8.2 +/- 1.6% vs. 6 +/- 1.3%, p < 0.001). Endothelium-independent responses to nitroglycerin were unchanged. No adverse events were observed.
CONCLUSIONS:
Folic acid supplementation improves arterial endothelial function in adults with relative hyperhomocystinemia, with potentially beneficial effects on the atherosclerotic process.
Am J Clin Nutr. 2015 Mar;101(3):646-58.
High folic acid consumption leads to pseudo-MTHFR deficiency, altered lipid metabolism, and liver injury in mice.[Pubmed:
25733650]
Increased consumption of Folic acid is prevalent, leading to concerns about negative consequences. The effects of Folic acid on the liver, the primary organ for folate metabolism, are largely unknown. Methylenetetrahydrofolate reductase (MTHFR) provides methyl donors for S-adenosylmethionine (SAM) synthesis and methylation reactions.
Our goal was to investigate the impact of high Folic acid intake on liver disease and methyl metabolism.
METHODS AND RESULTS:
Folic acid-supplemented diet (FASD, 10-fold higher than recommended) and control diet were fed to male Mthfr(+/+) and Mthfr(+/-) mice for 6 mo to assess gene-nutrient interactions. Liver pathology, folate and choline metabolites, and gene expression in folate and lipid pathways were examined.
Liver and spleen weights were higher and hematologic profiles were altered in FASD-fed mice. Liver histology revealed unusually large, degenerating cells in FASD Mthfr(+/-) mice, consistent with nonalcoholic fatty liver disease. High Folic acid inhibited MTHFR activity in vitro, and MTHFR protein was reduced in FASD-fed mice. 5-Methyltetrahydrofolate, SAM, and SAM/S-adenosylhomocysteine ratios were lower in FASD and Mthfr(+/-) livers. Choline metabolites, including phosphatidylcholine, were reduced due to genotype and/or diet in an attempt to restore methylation capacity through choline/betaine-dependent SAM synthesis. Expression changes in genes of one-carbon and lipid metabolism were particularly significant in FASD Mthfr(+/-) mice. The latter changes, which included higher nuclear sterol regulatory element-binding protein 1, higher Srepb2 messenger RNA (mRNA), lower farnesoid X receptor (Nr1h4) mRNA, and lower Cyp7a1 mRNA, would lead to greater lipogenesis and reduced cholesterol catabolism into bile.
CONCLUSIONS:
We suggest that high Folic acid consumption reduces MTHFR protein and activity levels, creating a pseudo-MTHFR deficiency. This deficiency results in hepatocyte degeneration, suggesting a 2-hit mechanism whereby mutant hepatocytes cannot accommodate the lipid disturbances and altered membrane integrity arising from changes in phospholipid/lipid metabolism. These preliminary findings may have clinical implications for individuals consuming high-dose Folic acid supplements, particularly those who are MTHFR deficient.