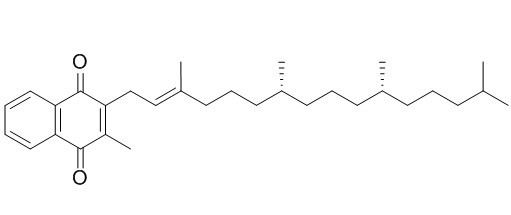
Vitamin K1
Vitamin K1, a fat-soluble, naturally occurring vitamin required for blood coagulation and bone and vascular metabolism. Vitamin K1 has anticoagulation activity, it may attenuate liver fibrosis by inhibiting hepatic stellate cell activation in bile duct-ligated rats; it inhibits diabetic-cataract by modulating lens Ca2+ homeostasis and its hypoglycemic effect through its direct action on the pancreas.Vitamin K1 may substantially contribute to reducing postmenopausal bone loss at the site of the femoral neck.
Inquire / Order:
manager@chemfaces.com
Technical Inquiries:
service@chemfaces.com
Tel:
+86-27-84237783
Fax:
+86-27-84254680
Address:
1 Building, No. 83, CheCheng Rd., Wuhan Economic and Technological Development Zone, Wuhan, Hubei 430056, PRC
Providing storage is as stated on the product vial and the vial is kept tightly sealed, the product can be stored for up to
24 months(2-8C).
Wherever possible, you should prepare and use solutions on the same day. However, if you need to make up stock solutions in advance, we recommend that you store the solution as aliquots in tightly sealed vials at -20C. Generally, these will be useable for up to two weeks. Before use, and prior to opening the vial we recommend that you allow your product to equilibrate to room temperature for at least 1 hour.
Need more advice on solubility, usage and handling? Please email to: service@chemfaces.com
The packaging of the product may have turned upside down during transportation, resulting in the natural compounds adhering to the neck or cap of the vial. take the vial out of its packaging and gently shake to let the compounds fall to the bottom of the vial. for liquid products, centrifuge at 200-500 RPM to gather the liquid at the bottom of the vial. try to avoid loss or contamination during handling.
Antioxidants (Basel).2023, 12(7):1324.
In Vitro Cellular & Developmental Biology - Plant2022, 58:972-988.
Phytochemistry Letters2021, 43:80-87.
J Food Sci Technol.2022, 59(1):212-219.
LWT2021, 147:111620.
Aquaculture2019, 510:392-399
Int J Mol Sci.2023, 24(4):3682.
Int J Mol Sci.2022, 23(11):6172.
J Adv Res.2021, 35:245-257.
Nat Prod Sci.2016, 22(2)
Related and Featured Products
J Biol Chem. 2014 Oct 31;289(44):30743-52.
Intestinal scavenger receptors are involved in vitamin K1 absorption.[Pubmed:
25228690]
Vitamin K1 (phylloquinone) intestinal absorption is thought to be mediated by a carrier protein that still remains to be identified.
METHODS AND RESULTS:
Apical transport of Vitamin K1 was examined using Caco-2 TC-7 cell monolayers as a model of human intestinal epithelium and in transfected HEK cells. Vitamin K1 uptake was then measured ex vivo using mouse intestinal explants. Finally, Vitamin K1 absorption was compared between wild-type mice and mice overexpressing scavenger receptor class B type I (SR-BI) in the intestine and mice deficient in cluster determinant 36 (CD36). Vitamin K1 uptake by Caco-2 cells was saturable and was significantly impaired by co-incubation with α-tocopherol (and vice versa). Anti-human SR-BI antibodies and BLT1 (a chemical inhibitor of lipid transport via SR-BI) blocked up to 85% of Vitamin K1 uptake. BLT1 also decreased Vitamin K1 apical efflux by ~80%. Transfection of HEK cells with SR-BI and CD36 significantly enhanced Vitamin K1 uptake, which was subsequently decreased by the addition of BLT1 or sulfo-N-succinimidyl oleate (CD36 inhibitor), respectively. Similar results were obtained in mouse intestinal explants. In vivo, the Vitamin K1 postprandial response was significantly higher, and the proximal intestine mucosa Vitamin K1 content 4 h after gavage was increased in mice overexpressing SR-BI compared with controls. Vitamin K1 postprandial response was also significantly increased in CD36-deficient mice compared with wild-type mice, but their Vitamin K1 intestinal content remained unchanged.
CONCLUSIONS:
Overall, the present data demonstrate for the first time that intestinal scavenger receptors participate in the absorption of dietary Vitamin K1.
Exp Eye Res. 2014 Nov;128:73-82.
Inhibition of diabetic-cataract by vitamin K1 involves modulation of hyperglycemia-induced alterations to lens calcium homeostasis.[Pubmed:
25257692]
This study investigated the potential of Vitamin K1 against streptozotocin-induced diabetic cataract in Wistar rats.
METHODS AND RESULTS:
A single, intraperitoneal injection of streptozotocin (STZ) (35 mg/kg) resulted in hyperglycemia, accumulation of sorbitol and formation of advanced glycation end product (AGE) in eye lens. Hyperglycemia in lens also resulted in superoxide anion and hydroxyl radical generation and less reduced glutathione suggesting oxidative stress in lens. Hyperglycemia also resulted in increase in lens Ca2+ and significant inhibition of lens Ca2+ ATPase activity. These changes were associated with cataract formation in diabetic animals. By contrast treatment of diabetic rats with Vitamin K1 (5 mg/kg, sc, twice a week) resulted in animals with partially elevated blood glucose and with transparent lenses having normal levels of sorbitol, AGE, Ca2+ ATPase, Ca2+, and oxidative stress. Vitamin K 1 may function to protect against cataract formation in the STZ induced diabetic rat by affecting the homeostasis of blood glucose and minimizing subsequent oxidative and osmotic stress.
METHODS AND RESULTS:
Thus, these results show that Vitamin K1 inhibits diabetic-cataract by modulating lens Ca2+ homeostasis and its hypoglycemic effect through its direct action on the pancreas.
Scand J Gastroenterol. 2014 Jun;49(6):715-21.
Vitamin K1 attenuates bile duct ligation-induced liver fibrosis in rats.[Pubmed:
24742111]
Vitamin K1 is used as a liver protection drug for cholestasis-induced liver fibrosis in China, but the mechanism of Vitamin K1's action in liver fibrosis is unclear.
METHODS AND RESULTS:
In this study, a model of liver fibrosis was achieved via bile duct ligation in rats. The rats were then injected with Vitamin K1, and the levels of serum aspartate aminotransferase, alanine transaminase, total bilirubin and the fibrotic grade score, collagen content, the expressions of α-smooth muscle actin (SMA) and cytokeratin 19 (CK19) were measured on day 28 after ligation. The levels of the biochemical parameters, fibrotic score and collagen content were significantly reduced by treatment with Vitamin K1 in bile duct-ligated rats. In addition, α-SMA and CK19 expression was significantly reduced by Vitamin K1 treatment in bile duct-ligated rats.
CONCLUSIONS:
These results suggested that Vitamin K1 may attenuate liver fibrosis by inhibiting hepatic stellate cell activation in bile duct-ligated rats.
Nephrol Dial Transplant. 2014 Sep;29(9):1633-8.
Vitamin K1 to slow vascular calcification in haemodialysis patients (VitaVasK trial): a rationale and study protocol.[Pubmed:
24285427]
Patients on haemodialysis (HD) exhibit increased cardiovascular mortality associated with accelerated vascular calcification (VC). VC is influenced by inhibitors such as matrix Gla protein (MGP), a protein activated in the presence of vitamin K. HD patients exhibit marked vitamin K deficiency, and supplementation with vitamin K reduces inactive MGP levels in these patients. The VitaVasK trial analyses whether Vitamin K1 supplementation affects the progression of coronary and aortic calcification in HD patients.
METHODS AND RESULTS:
VitaVasK is a prospective, randomized, parallel group, multicentre trial (EudraCT No.: 2010-021264-14) that will include 348 HD patients in an open-label, two-arm design. After baseline multi-slice computed tomography (MSCT) of the heart and thoracic aorta, patients with a coronary calcification volume score of at least 100 will be randomized to continue on standard care or to receive additional supplementation with 5 mg Vitamin K1 orally thrice weekly. Treatment duration will be 18 months, and MSCT scans will be repeated after 12 and 18 months. Primary end points are the progression of thoracic aortic and coronary artery calcification (calculated as absolute changes in the volume scores at the 18-month MSCT versus the baseline MSCT). Secondary end points comprise changes in Agatston score, mitral and aortic valve calcification as well as major adverse cardiovascular events (MACE) and all-cause mortality. VitaVask also aims to record MACE and all-cause mortality in the follow-up period at 3 and 5 years after treatment initiation.
CONCLUSIONS:
This trial may lead to the identification of an inexpensive and safe treatment or prophylaxis of VC in HD patients.
Calcif Tissue Int. 2003 Jul;73(1):21-6.
Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age.[Pubmed:
14506950]
Although several observational studies have demonstrated an association between vitamin K status and bone mineral density (BMD) in postmenopausal women, no placebo-controlled intervention trials of the effect of Vitamin K1 supplementation on bone loss have been reported thus far.
METHODS AND RESULTS:
In the trial presented here we have investigated the potential complementary effect of Vitamin K1 (1 mg/day) and a mineral + vitamin D supplement (8 microg/day) on postmenopausal bone loss. The design of our study was a randomized, double-blind, placebo-controlled intervention study; 181 healthy postmenopausal women between 50 and 60 years old were recruited, 155 of whom completed the study. During the 3-year treatment period, participants received a daily supplement containing either placebo, or calcium, magnesium, zinc, and vitamin D (MD group), or the same formulation with additional Vitamin K1 (MDK group). The main outcome was the change in BMD of the femoral neck and lumbar spine after 3 years, as measured by DXA. The group receiving the supplement containing additional Vitamin K1 showed reduced bone loss of the femoral neck: after 3 years the difference between the MDK and the placebo group was 1.7% (95% Cl: 0.35-3.44) and that between the MDK and MD group was 1.3% (95% Cl: 0.10-3.41). No significant differences were observed among the three groups with respect to change of BMD at the site of the lumbar spine.
CONCLUSIONS:
If co-administered with minerals and vitamin D, Vitamin K1 may substantially contribute to reducing postmenopausal bone loss at the site of the femoral neck.
Mayo Clin Proc. 2001 Mar;76(3):260-6.
Efficacy and safety of intravenous phytonadione (vitamin K1) in patients on long-term oral anticoagulant therapy.[Pubmed:
11243272 ]
To determine the safety and efficacy of intravenously administered phytonadione (Vitamin K1) in patients on routine oral warfarin anticoagulation.
METHODS AND RESULTS:
This retrospective cohort study comprised adults who were taking warfarin, were not bleeding, and received intravenous phytonadione anticoagulation therapy before a diagnostic or therapeutic procedure between September 1, 1994, and March 31, 1996. The main outcome measures were adverse reactions to intravenously administered phytonadione, prothrombin-international normalized ratio time values, the incidence of bleeding and thrombosis after the procedure, and the time between the procedure and return to anticoagulation after resumption of warfarin treatment.
Two (1.9%) of the 105 patients studied had suspected adverse reactions to intravenous phytonadione (dyspnea and chest tightness during infusion in both). For the 82 patients who underwent a procedure, the median time from phytonadione to procedure onset was 27 hours (range, 0.7-147 hours), which was significantly less for patients receiving an initial phytonadione dose of more than 1 mg (P=.009). None had thromboembolism after surgery, although 2 (2.4%) of the 82 patients had procedure-associated major bleeding. For the 60 patients resuming warfarin therapy after a procedure, the median time to return to therapeutic anticoagulation was 4.1 days (range, 0.8-31.7 days) and was unaffected by the phytonadione dosage.
CONCLUSIONS:
Intravenous phytonadione appears to be safe and is effective for semiurgent correction of long-term oral anticoagulation therapy before surgery. In small doses, it does not prolong the patient's time to return to therapeutic anticoagulation.
PLoS One. 2014 Mar 4;9(3):e90199.
The severe adverse reaction to vitamin k1 injection is anaphylactoid reaction but not anaphylaxis.[Pubmed:
24594861]
The severe adverse reaction to Vitamin K1 injection is always remarkable and is thought to result from anaphylaxis. Paradoxically, however, some patients administered Vitamin K1 injection for the first time have adverse reactions.
METHODS AND RESULTS:
Using beagle dogs, the present study tested the hypothesis that the response to Vitamin K1 is an anaphylactoid reaction. The results showed that serious anaphylaxis-like symptoms appeared in beagle dogs after the administration of Vitamin K1 injection for the first time. The plasma histamine concentration increased, and blood pressure decreased sharply. After sensitization, dogs were challenged with Vitamin K1 injection and displayed the same degree of symptoms as prior to sensitization. However, when the Vitamin K1 injection-sensitized dogs were challenged with a Vitamin K1-fat emulsion without solubilizers such asTween-80, the abnormal reactions did not occur. Furthermore, there was no significant change in the plasma immunoglobulin E concentration after Vitamin K1 challenge. Following treatment with Vitamin K1 injection, the release of histamine and β-hexosaminidase by rat basophilic leukemia-2H3 cells as well as the rate of apoptosis increased. The Tween-80 group displayed results similar to those observed following Vitamin K1 injection in vivo. However, the dogs in the Vitamin K1-fat emulsion group did not display any abnormal behavior or significant change in plasma histamine. Additionally, degranulation and apoptosis did not occur in rat basophilic leukemia-2H3 cells.
CONCLUSIONS:
Our results indicate that the adverse reaction induced by Vitamin K1 injection is an anaphylactoid reaction, not anaphylaxis. Vitamin K1 injection induces the release of inflammatory factors via a non-IgE-mediated immune pathway, for which the trigger may be the solubilizer.